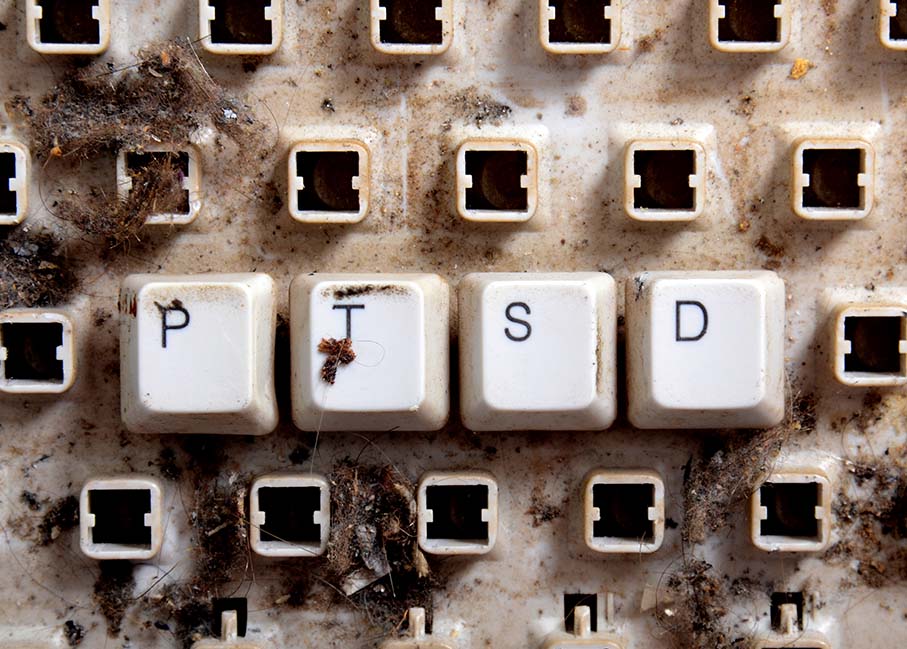
Reacting to a Traumatic Event
It’s not unusual for people who have experienced traumatic events to have flashbacks, nightmares, or intrusive memories when something terrible happens — like the 9/11 terrorist attacks and those in cities around the world (Orlando and Paris, for example) or the bombings at the 2013 Boston Marathon, or active combat.
Be tolerant of your nervous system: It’s having a normal reaction. Try not to get hooked to news reports, which may seem particularly compelling. Spend time with loved ones in favorite activities or outside in nature, and avoid alcohol.
Learn more below, including how to help children.
Most people who experience such events recover from them, but people with PTSD continue to be severely depressed and anxious for months or even years following the event.
Women are twice as likely to develop posttraumatic stress disorder as men, and children can also develop it. PTSD often occurs with depression, substance abuse, or other anxiety disorders.
PTSD Symptoms
PTSD is diagnosed after a person experiences symptoms for at least one month following a traumatic event. However symptoms may not appear until several months or even years later. The disorder is characterized by three main types of symptoms:
- Re-experiencing the trauma through intrusive distressing recollections of the event, flashbacks, and nightmares.
- Emotional numbness and avoidance of places, people, and activities that are reminders of the trauma.
- Increased arousal such asinsomnia, difficulty and concentrating, feeling jumpy, and being easily irritated and angered.
Diagnosis criteria that apply to adults, adolescents, and children older than six include those below.
Exposure to actual or threatened death, serious injury, or sexual violation:
- directly experiencing the traumatic events
- witnessing the traumatic events in person,
- learning that the traumatic events occurred to a close family member or close friend; cases of actual or threatened death must have been violent or accidental
- experiencing repeated or extreme exposure to aversive details of the traumatic events (Examples are first responders collecting human remains; police officers repeatedly exposed to details of child abuse). Note: This does not apply to exposure through electronic media, television, movies, or pictures, unless exposure is work-related.
The presence of one or more of the following:
- spontaneous or cued recurrent, involuntary, and intrusive distressing memories of the traumatic events (Note: In children repetitive play may occur in which themes or aspects of the traumatic events are expressed.)
- recurrent distressing dreams in which the content or affect (i.e. feeling) of the dream is related to the events (Note: In children there may be frightening dreams without recognizable content.)
- flashbacks or other dissociative reactions in which the individual feels or acts as if the traumatic events are recurring (Note: In children trauma-specific reenactment may occur in play.)
- intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic events
- physiological reactions to reminders of the traumatic events
Persistent avoidance of distressing memories, thoughts, or feelings about or closely associated with the traumatic events or of external reminders (i.e., people, places, conversations, activities, objects, situations)
Two or more of the following:
- inability to remember an important aspect of the traumatic events (not due to head injury, alcohol, or drugs)
- persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” “The world is completely dangerous”).
- persistent, distorted blame of self or others about the cause or consequences of the traumatic events
- persistent fear, horror, anger, guilt, or shame
- markedly diminished interest or participation in significant activities
- feelings of detachment or estrangement from others
- persistent inability to experience positive emotions
Two or more of the following marked changes in arousal and reactivity:
- irritable or aggressive behavior
- reckless or self-destructive behavior
- hypervigilance
- exaggerated startle response
- problems with concentration
- insomnia
Also, clinically significant distress or impairment in social, occupational, or other important areas of functioning not attributed to the direct physiological effects of medication, drugs, or alcohol or another medical condition, such as traumatic brain injury.
Relationships, Trauma, and PTSD
Trauma survivors who have PTSD may have trouble with their close family relationships or friendships. Their symptoms can cause problems with trust, closeness, communication, and problem solving, which may affect the way the survivor acts with others. In turn, the way a loved one responds to him or her affects the trauma survivor. A circular pattern may develop that could harm relationships.
PTSD Facts
- 7.7 million Americans age 18 and older have PTSD.
- 67 percent of people exposed to mass violence have been shown to develop PTSD, a higher rate than those exposed to natural disasters or other types of traumatic events.
- People who have experienced previous traumatic events run a higher risk of developing PTSD.